Steelers wide receiver George Pickens popped up on the injury report last Friday prior the Steelers’ second meeting with the Cleveland Browns. Friday practices are usually not that physical, and it was later revealed that the injury occurred late in practice on Thursday. Initially, it didn’t sound serious. He was listed as “questionable” for his game status. With the league’s removal of the “probable” designation, that was the best-case scenario.
Head coach Mike Tomlin expressed optimism that Pickens would be able to play. Reports detailed a plan for Pickens to test his hamstring in pregame warmups. Instead, Pickens was ruled out and sideline reporters noted that Pickens was never seen on the field prior to that.
Following the Steelers’ 27-14 win over the Browns, Tomlin clarified the reason why Pickens couldn’t play. It basically came down to not wanting to run the risk of aggravating the injury. On Monday, the Pittsburgh Post-Gazette’s Gerry Dulac reported that Pickens was likely to miss the Steelers’ upcoming game against the Philadelphia Eagles with a Grade 2 hamstring injury. This was also reported by NFL Insider Adam Schefter on The Pat McAfee Show.
During his weekly press conference on Tuesday, Tomlin added further detail:
- Pickens experienced some hamstring discomfort post-practice last Thursday while getting some extra work in.
- Pickens felt pretty good on Friday but was limited to save him for Sunday.
- The plan was to see how Pickens felt and looked in pregame warmups. If he played, it would be on a snap count to save him for “weighty downs.”
- Pickens woke up Sunday feeling more discomfort, so he was held out of the game.
- An MRI taken Monday showed that the injury was a little more significant than originally expected.
- Pickens is currently considered doubtful and probably out for the Eagles game on Sunday.
So how serious is George Pickens’s hamstring injury and how much time will the Steelers WR1 miss?
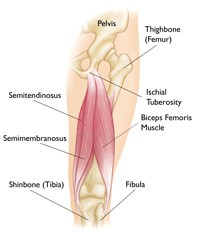
As always, we need to start with the anatomy. The hamstring is actually 3 muscles, the semitendinosus, semimembranosus, and the biceps femoris:
| They start at the bottom of the pelvis at a place called the ischial tuberosity. They cross the knee joint and end at the lower leg. Hamstring muscle fibers join with the tough, connective tissue of the hamstring tendons near the points where the tendons attach to bones. The hamstring-muscle group helps you extend your leg straight back and bend your knee. | |
Fun fact: The origin of the word hamstring comes from the old English hamm, meaning thigh. String refers to the characteristic appearance and feel of the tendons just above the back of the knee.
Here is an MRI image of the anatomy:
Hamstring injuries occur most frequently in sports that require athletes to sprint with sudden starts and stops. From the AAOS: During sprinting, the hamstring muscles contract eccentrically as the back leg is straightened and the toes are used to push off and move forward. The hamstring muscles are not only lengthened at this point in the stride, but they are also loaded — with body weight as well as the force required for forward motion.
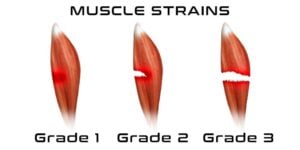
Like many injuries, hamstring strains are classified by grade. Unlike other injuries, it isn’t very scientific. This is from an Aussie physiotherapist:
- Grade 1 Hamstring Strain: With a Grade 1 hamstring strain you may have tightness in back of the thigh but will be able to walk normally. You will be aware of some hamstring discomfort and unable to run at full speed. There will be mild swelling and spasm. Bend your knee against resistance is unlikely to reproduce much pain.
- Grade 2 Hamstring Strain: With a Grade 2 hamstring strain your walking pattern will be affected and you will most likely be limping. Sudden twinges of hamstring pain during activity will be present. You may notice some hamstring muscle swelling and your hamstring will be tender to palpate. It will also be painful for you to bend your knee against resistance.
- Grade 3 Hamstring Strain: A Grade 3 hamstring strain is a severe injury involving a tear to half or all of the hamstring muscle. You may need crutches to walk and will feel severe pain and weakness in the muscle. Swelling will be noticeable immediately and bruising will usually appear within 24 hours.
Grade 3 injuries can involve a full separation of the muscle from the pelvis, where the tendon can actually cause an avulsion of the pubic bone. This results in a “popping” sensation and a nasty-looking wad of muscle on the back of the thigh.
The simple depiction of hamstring-injury grades:
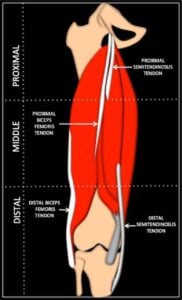
But it’s actually more complicated than that. Because some hamstring injuries involve pure muscle tears and others are due to tendon tears and how proximal or distal along the thigh is also a factor:
An MRI is probably the best way to define hamstring injuries, which are graded by the radiologist based on:
- The muscles or tendons involved (semimembranosus, biceps femoris short, biceps femoris long head, semitendinosus).
- The location of involvement for each muscle or tendon (muscle belly or muscle/tendon junction).
- The cross-sectional percentage of involvement (0, 25, 50, 75, 100).
- The amount of tendon or muscle retraction in centimeters.
- Any signs of chronic muscle or tendon damage.
- The overall length on the damage along the muscle.
TREATMENT
Treatment includes the traditional RICE (rest, ice, compression, and elevation). After the swelling decreases, sports massage and ultrasound therapy can be used as well as foam-roller exercises to promote myofascial release to the muscles. Once the acute phase is passed, stretching and strengthening exercises are done but only if pain free. Eventually, the player will progress to more dynamic and functional exercise and finally graduate to football-specific drills.
How long this process takes depends, of course, on the extent of the muscle and tendon damage sustained. Plasma-rich protein (PRP) injections are sometimes used for acute hamstring injuries to reduce recovery time.
MEDICAL DATA
Pittsburgh’s own Dr. James Bradley and colleagues looked at the use of MRI on hamstring injuries in professional football players to predict return to play. Using standard radiology grading of hamstring injuries, they looked at 38 players with a total of 43 injuries (some were bilateral and recurrences were also included). They developed an MRI score based on player age at the time of injury, number of muscles involved, location of injury, insertional injury, percentage of muscle injured, retraction of muscle or tendon, and length of long axis T2 signal.
They also analyzed the MRI grade by games missed:
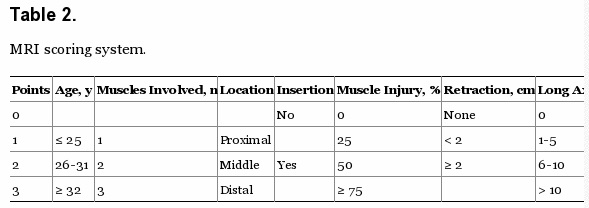  |
Including all players and all injury severities, an average of 11.3 practices and 2.6 games were missed. In 10 cases, no games were missed and in another 10 cases, only one game was missed. In 14 cases, two or three games were missed, and in nine cases, at least four games were missed.
Here is what they concluded: After acute hamstring strain, players had a longer recovery when they were found to have multiple muscle/tendon involvement, a high percentage of muscle involvement (over 75 percent), long T2 sagittal plane signal (over 10 cm), and retraction. They determined that MRIs are reliable in determining severity of injury and time away from sport for hamstring injuries in professional football players.
A more recent British study of elite football (soccer) players in both the Premier League and the Championship League looked at whether the type of hamstring injury impacted the return to play. Injuries were classified using the British Athletics Muscle Injury Classification:
In a review of 61 hamstring injuries, the investigators found:
- The intramuscular tendon was injured in 21 percent of cases.
- Return to full training was faster in cases without intramuscular tendon injury (24 days) than in cases with intramuscular tendon injury (36 days).
- Reinjury rate was higher in cases with intramuscular tendon injury (38.5 percent) than cases without intramuscular tendon injury (12.5 percent).
Just five days ago, a 12-year review of hamstring injuries in the NFL database from 2008-2020 was published in the Orthopaedic Journal of Sports Medicine. Here is what they found:
- 2.101 hamstring injuries were sustained 1,354 players.
- The mean duration on the injury report was 2.4 weeks, which included DNP, limited and full participation.
- 33 percent of players suffered reinjury, with 27 percent of those in the same season.
- There was no difference in return to play for players with or without reinjury.
- Hamstring injuries were more common in defensive skill players (50.4 percent) than offensive skill players (37.7 percent).
To this day, my favorite example of an athlete sharing medical information has to be when Arian Foster tweeted his MRI and noted the “anti-awesomeness” on his hamstring back in 2011.
Although Foster was sure he would play in Week 1, his missed the season opener two weeks after his initial injury. He played Week 2 and re-aggravated the injury. He returned again in Week 4 and was able to play the rest of the season.
DOES PRP HELP?
In 2020, Dr. James Bradley published a study on platelet-rich plasma use in NFL players with acute hamstring injuries. Sixty-nine NFL players from a single team (pretty good bet that was the Steelers) who sustained acute Grade 2 hamstring injuries, as diagnosed via MRI from 2009 to 2018, were retrospectively reviewed. Average days, practices, and games missed were recorded. Players who did and did not receive PRP (leukocyte-poor) injections were compared. Those who received PRP did so within 24-to-48 hours after injury.
His data showed that PRP injections for acute Grade 2 hamstring injuries in NFL players showed no significant difference in days missed or time to return to practice but did allow for faster return to play, with a one game overall difference:
- Average time missed in those treated with PRP injections was 22.5 days, 18.2 practices, and 1.3 games.
- For those who did not receive PRP injections, time missed was 25.7 days (P = .81), 22.8 practices (P = .68), and 2.9 games
Given that Dr. Bradley is the head orthopaedic surgeon for the Steelers, it is possible that George Pickens will be treated with PRP in get him back onto the field faster.
SO WHEN WILL PICKENS BE BACK?
Not knowing what the MRI showed, the level of the injury, and whether Pickens has tendon involvement, it’s hard to give a solid prediction. As Tomlin always says, his participation in practice will be the Steelers’ guide. It’s very likely that Pickens will miss the Eagles game this Sunday.
The big question is whether he can make it back for the Ravens game on Dec. 21. The Steelers have been conservative managing players with hamstring injuries this season. With the team heading to Baltimore just six days after they travel to Philadelphia, it is possible that Pickens will remain on the sideline even if he makes the trip. While Tomlin won’t rush a player back who isn’t ready, the outcome of the Ravens game could determine the AFC North champion and a home game in the first round of the playoffs.
Based on the data, and the possibility that he might be getting treated with PRP, George Pickens could be ready by then. And after watching this week’s Hard Knocks, it’s clear Pickens wants to be back on the field already.
Melanie H. Friedlander, M.D., F.A.C.S. is a doctor at Association of South Bay Surgeons in Torrance, California. Dr. Friedlander enjoys all aspects of general surgery, but her primary areas of focus are breast surgery and advanced laparoscopic surgery. She recently adopted an advanced, minimally invasive technique that reduces scar size in thyroid surgery. Dr. Friedlander is a member of the Society of American Gastrointestinal Endoscopic Surgeons (SAGES) and the Society of Laparoscopic Surgeons. She developed and published many scientific studies in highly esteemed medical journals.