It was a bittersweet victory for the Steelers and their fans, as the team finally scored their first home win of the season but lost their star WR JuJu Smith-Schuster in the second quarter after a huge hit by Broncos safety Kareem Jackson. After a brief evaluation on the sidelines that served only to establish how much pain JuJu was experiencing, he was led to the locker room and eventually to the hospital. He was seen the following night at his charity event in a right arm sling and Head Coach Mike Tomlin confirmed during his Tuesday media session that JuJu would have surgery on Wednesday. We know from his IG account that his surgery was a success.
So what exactly is JuJu’s injury? Both Ian Rapoport and Adam Schefter tweeted that JuJu had his dislocated right shoulder reduced at the hospital after the game. Rapoport later clarified that JuJu would need surgery as well:
Knowing this and looking at the game film again, I would guess this is how it played out:
- Jackson’s hit on JuJu probably caused the dislocation.
- JuJu landed on his outstretched right arm with his shoulder dislocated, likely worsening any ligament damage.
- The trainers tried moving JuJu’s arm on the sideline, causing serious pain because it was still dislocated.
- The medical staff was unable to reduce the dislocated shoulder in the locker room and JuJu was transported to the hospital to have this done, possibly under sedation (which may have caused the confusion that led to Rapoport’s initial incorrect report that JuJu had already had surgery).
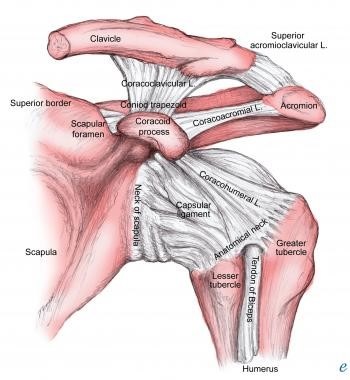
So as always, I will make the disclaimer that I have no verified information on JuJu’s injury and no access to his records. Now let’s look at some shoulder anatomy:
The shoulder joint is made by the junction of three bones: the collarbone (clavicle), the shoulder blade (scapula), and the upper arm bone (humerus). The rounded end of the humerus sits in this joint like a ball in a socket and is held in place by a variety of ligaments:
If the humeral head is forcefully moved out of the socket, that is considered a dislocation.
- Anterior (forward). The head of the humerus is moved forward out of the socket. This is the most common type of dislocation (95% of the general population) and usually happens when the arm is extended.
- Posterior (behind). The head of the humerus is moved behind and above the socket. This is a less common type of dislocation.
- Inferior (bottom). The head of the humerus is forced down and out of the socket toward the armpit. This is the least common type of dislocation.
Shoulder subluxation is a partial or incomplete dislocation of the shoulder joint caused by weakness of rotator cuff muscles or laxity of the shoulder ligaments causes the “ball” to slip out of the “socket”. This usually reduces or pops back in by itself.
Here you can see an Xray image of an anterior dislocation:
Figure 1 radiopaedia.org
Most data shows that NFL players return to play (RTP) in 0-3 weeks after a shoulder subluxation or dislocation.
In a review of 83 NFL players who sustained an in-season shoulder instability event while playing in the NFL, overall RTP was determined, and players who did and did not undergo operative repair were compared. This study found that players who avoided surgery had a RTP of 0-3 weeks and RTP for players who had surgery was a median of 39.3 weeks. Players who underwent surgery had a lower recurrence rate and a longer interval to the recurrence if it occurred.
In another study, the NFL’s injury database was reviewed for shoulder instability injuries resulting in missed time from 2012 to 2017. During the 6-year study period, 355 players sustained 403 missed-time shoulder instability injuries.
- 70% of injuries were subluxations and 30% were dislocations.
- 75% of dislocations were anterior, while subluxations were more evenly distributed between the anterior and posterior directions (45% vs 52%, respectively).
- Players missed substantially more time after dislocation compared with subluxation (median, 47 days vs 13 days, respectively).
- When instability direction was known, the majority of instability events among quarterbacks and offensive linemen were posterior (73% and 53%, respectively), while anterior instability was most common for all other positions.
Here’s the breakdown by position and type of shoulder instability:
In a different review of the NFL database from 2000 to 2019 that looked only at players with their first episode of shoulder instability, the authors found:
- Athletes who RTP in the NFL after a shoulder instability injury do so with a similar workload and performance irrespective of surgical or nonsurgical management.
- Nonoperative treatment is associated with faster RTP.
- Operative management is associated with fewer recurrent instability events, greater time between recurrent instability events, and greater career longevity.
So what was the urgency for JuJu’s surgery? He must have had associated ligament injuries, as speculated by Dr. David Chao and also suggested by Ian Rapoport, who mentioned the possibility of a labral tear in his tweet.
A number of associated injuries may be sustained at the time of the shoulder dislocation. Bankart and Hill-Sachs lesions (mentioned by Dr. Chao) result from an anterior shoulder dislocation.
A Bankart lesion is an avulsion or tearing away of the labrum from the rim of the “socket”, whereas a Bony Bankart lesion is a fracture of the anteroinferior portion of the “socket” in conjunction with this labral injury. With a Hill-Sachs lesion, the humeral head ‘collides’ with the anterior part of the socket, causing bone loss, a cartilage defect and deformity of the humeral head. Other associated ligament and bony injuries as well as capsular avulsions may occur. Here’s a short video depicting Bankart and Hill-Sachs injuries.
In a 2012 study, Owens et al. published a comprehensive review on the management of midseason traumatic anterior shoulder instability in athletes. They found that osseous (bony) defects >25% on imaging correlated with a higher rate of recurrent instability and predicted a poor outcome with nonsurgical management. They also recommended that nonoperative in-season management be reserved for “noncontact and nonthrowing athletes.”
Most likely, JuJu’s orthopaedic surgeon strongly recommended surgery based on the extent of injury to his shoulder ligaments and the high likelihood of recurrent shoulder instability, either this season or in the future. Knowing how hard JuJu worked to be in perfect shape this season, his commitment to the team and the fact that this is a contract year for him, this was probably a crushing decision but the right one for his future. Here’s wishing him a speedy recovery and that somehow, some way, that future is in Pittsburgh.
“Melanie H. Friedlander, M.D., F.A.C.S. is a doctor at Association of South Bay Surgeons in Torrance, California. Dr. Friedlander enjoys all aspects of general surgery, but her primary areas of focus are breast surgery and advanced laparoscopic surgery. She recently adopted an advanced, minimally invasive technique that reduces scar size in thyroid surgery. Dr. Friedlander is a member of the Society of American Gastrointestinal Endoscopic Surgeons (SAGES) and the Society of Laparoscopic Surgeons. She developed and published many scientific studies in highly esteemed medical journals.”